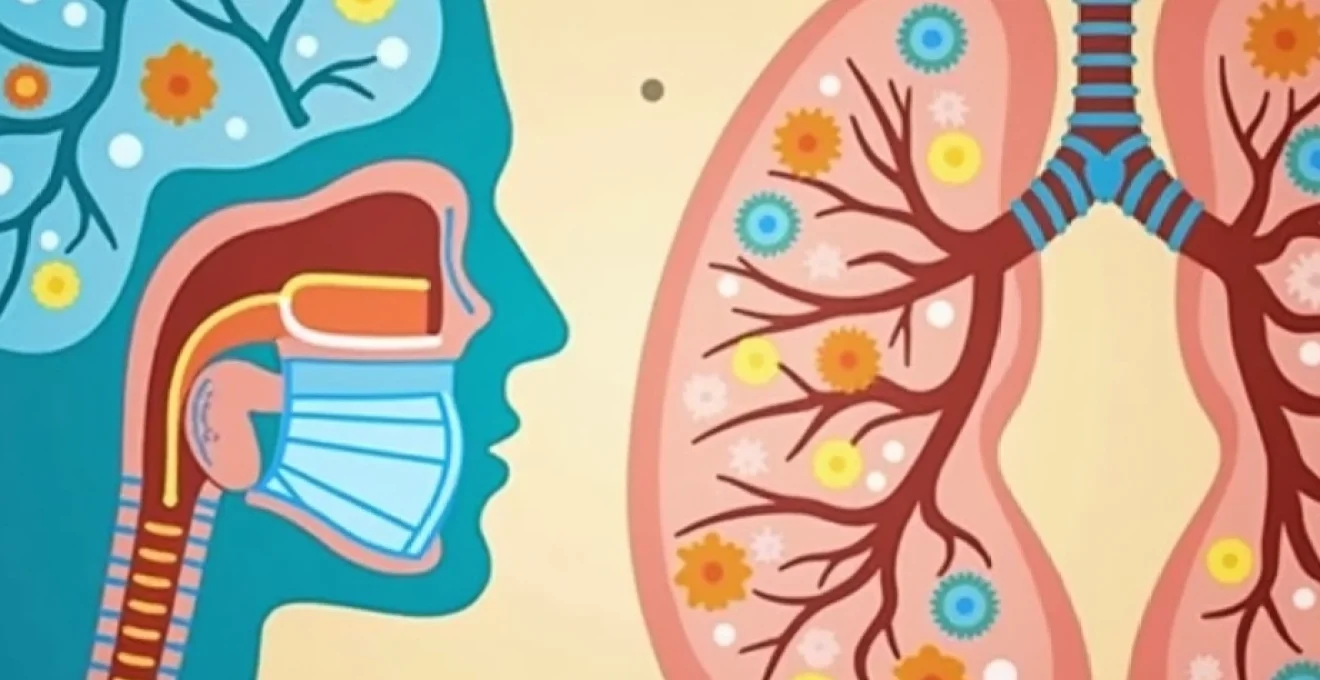
Millions of individuals worldwide experience acute bronchitis annually, often seeking relief from persistent coughing, chest congestion, and respiratory discomfort. Sudafed, containing the active ingredient pseudoephedrine hydrochloride, represents one of the most frequently considered over-the-counter medications for managing bronchitis-related symptoms. Understanding the relationship between this sympathomimetic decongestant and bronchial inflammation requires examining both the pathophysiology of acute bronchitis and the precise mechanisms through which pseudoephedrine operates within the respiratory system. The question of whether Sudafed provides meaningful relief for bronchitis symptoms involves complex pharmacological interactions that extend beyond simple nasal decongestion.
Pseudoephedrine hydrochloride mechanism of action in respiratory conditions
Pseudoephedrine hydrochloride functions as a potent sympathomimetic agent, targeting multiple adrenergic receptor subtypes throughout the respiratory tract to produce therapeutic effects. The medication’s primary mechanism involves both direct stimulation of adrenergic receptors and indirect effects through norepinephrine release from presynaptic storage sites. This dual-action approach enables pseudoephedrine to influence various aspects of respiratory physiology, from vascular tone to bronchial smooth muscle relaxation. Understanding these mechanisms provides crucial insight into how Sudafed might address specific bronchitis symptoms.
Alpha-adrenergic receptor stimulation and vasoconstriction effects
The alpha-adrenergic receptor activation by pseudoephedrine represents the foundation of its decongestant properties. When pseudoephedrine binds to alpha-1 adrenergic receptors in the respiratory mucosa, it triggers vasoconstriction of blood vessels supplying the nasal passages and upper respiratory tract. This vasoconstriction reduces blood flow to inflamed tissues, consequently decreasing mucosal swelling and edema formation. The reduction in tissue hyperemia directly contributes to improved airway patency and enhanced drainage of secretions from congested areas. For bronchitis patients experiencing upper respiratory involvement, this mechanism can provide relief from nasal stuffiness and facilitate better breathing patterns.
Nasal decongestant properties through sympathomimetic activity
The sympathomimetic activity of pseudoephedrine extends beyond simple vasoconstriction to encompass broader effects on respiratory tract physiology. Peak plasma concentrations of 180-300 ng/mL achieved within 1.39-2 hours following a 60mg dose correlate with optimal decongestant efficacy. The medication’s ability to reduce tissue congestion helps restore normal ciliary function, which becomes compromised during bronchitis episodes. Improved ciliary clearance facilitates the removal of excess mucus and inflammatory debris from the respiratory passages, potentially reducing the duration and severity of symptoms associated with acute bronchitis.
Bronchodilator potential via beta-2 receptor interaction
While primarily recognised for its decongestant properties, pseudoephedrine also demonstrates modest bronchodilatory effects through beta-2 adrenergic receptor stimulation. This mechanism involves the activation of adenyl cyclase, leading to increased cyclic adenosine monophosphate (cAMP) levels within bronchial smooth muscle cells. The elevation of cAMP concentrations promotes smooth muscle relaxation and bronchial dilation, though these effects remain less pronounced compared to dedicated bronchodilator medications. For bronchitis patients experiencing mild bronchoconstriction, this secondary effect may provide additional respiratory relief beyond simple decongestion.
Mucosal inflammation reduction in upper respiratory tract
Pseudoephedrine’s anti-inflammatory properties stem from its ability to reduce vascular permeability and limit inflammatory cell infiltration into respiratory tissues. The medication influences the release of inflammatory mediators, potentially moderating the intense mucosal inflammation characteristic of acute bronchitis. By stabilising vascular integrity and reducing capillary leak, pseudoephedrine helps maintain normal tissue architecture during the acute phase of bronchial infection. This stabilisation effect contributes to symptom resolution and may accelerate recovery from bronchitis episodes when used appropriately as part of comprehensive treatment strategies.
Acute bronchitis pathophysiology and symptom profile
Acute bronchitis develops through a complex cascade of inflammatory processes initiated primarily by viral pathogens affecting the bronchial tree. The condition involves inflammation of the large airways, specifically the bronchi, leading to characteristic symptoms including persistent cough, mucus production, and respiratory discomfort. Understanding the underlying pathophysiology helps explain why certain medications like Sudafed may provide symptom relief while highlighting the limitations of decongestant therapy in addressing the root causes of bronchitis. The inflammatory response involves multiple cellular and molecular mechanisms that contribute to the clinical presentation observed in affected individuals.
Viral aetiology including rhinovirus and respiratory syncytial virus
Viral infections account for approximately 90-95% of acute bronchitis cases, with rhinoviruses, respiratory syncytial virus, influenza viruses, and parainfluenza viruses representing the most common causative agents. These pathogens initially infect the upper respiratory tract before spreading to the bronchial epithelium, where they trigger localised inflammatory responses. The viral replication process damages ciliated epithelial cells, compromising normal mucociliary clearance mechanisms and predisposing patients to secondary bacterial infections. This viral aetiology explains why antibiotic therapy remains ineffective for most bronchitis cases, emphasising the importance of supportive care and symptomatic management approaches.
Inflammatory response in bronchial epithelium and mucosa
The inflammatory cascade in acute bronchitis involves recruitment of neutrophils, macrophages, and lymphocytes to the bronchial mucosa, resulting in tissue swelling and increased vascular permeability. Pro-inflammatory cytokines including interleukin-1β, tumour necrosis factor-α, and interleukin-6 orchestrate the immune response while contributing to symptom development. Epithelial cell damage exposes sensory nerve endings, triggering the persistent cough reflex characteristic of bronchitis. The inflammatory infiltrate also stimulates goblet cell hyperplasia and mucus gland hypertrophy, leading to excessive mucus production that further compromises airway function and perpetuates the cough cycle.
Mucus hypersecretion and ciliary dysfunction mechanisms
Acute bronchitis disrupts normal mucociliary escalator function through multiple mechanisms, including ciliary beat frequency reduction and altered mucus composition. The inflammatory response stimulates mucus-producing cells to increase secretion volume while simultaneously altering mucus viscosity and elasticity.
The combination of increased mucus production and impaired clearance creates the ideal conditions for persistent cough and chest congestion
that characterises acute bronchitis. This pathophysiological understanding helps explain why medications targeting mucus clearance or airway inflammation may provide more direct therapeutic benefit than simple decongestants for managing bronchitis symptoms.
Productive cough reflex and airway irritation patterns
The cough reflex in acute bronchitis results from increased sensitivity of irritant receptors located throughout the tracheobronchial tree. Inflammatory mediators lower the threshold for cough initiation while damaged epithelium exposes nerve endings to airway contents. The productive nature of bronchitis cough reflects attempts to clear excess secretions and inflammatory debris from the respiratory passages. Cough patterns typically evolve from initially dry and irritating to productive with purulent sputum as the condition progresses, often persisting for 2-3 weeks after other symptoms resolve due to ongoing airway inflammation and hypersensitivity.
Clinical evidence for sudafed efficacy in bronchitis management
The clinical evidence supporting pseudoephedrine use in acute bronchitis management remains limited and indirect, primarily derived from studies examining its effects on upper respiratory symptoms rather than specific bronchial inflammation. Most research has focused on pseudoephedrine’s decongestant properties in common cold and allergic rhinitis, with extrapolation to bronchitis symptoms based on overlapping pathophysiological mechanisms. Current clinical guidelines from the National Institute for Health and Care Excellence (NICE) do not specifically recommend pseudoephedrine for acute bronchitis, instead emphasising supportive care and symptom management through rest, hydration, and analgesics. However, some clinicians consider pseudoephedrine for bronchitis patients experiencing significant upper respiratory congestion that may contribute to overall symptom burden and recovery delay.
Observational studies suggest that pseudoephedrine may provide modest benefits for bronchitis patients who experience concurrent nasal congestion and sinus involvement, conditions that commonly accompany lower respiratory tract infections. The medication’s ability to improve upper respiratory drainage may indirectly benefit bronchial symptom resolution by reducing post-nasal drip and minimising cough triggers.
Clinical experience indicates that patients with mixed upper and lower respiratory symptoms may experience greater relief from combination therapy including decongestants
compared to those with isolated bronchial inflammation. However, controlled trials specifically examining pseudoephedrine efficacy in acute bronchitis remain scarce, limiting evidence-based recommendations for this indication.
The duration of symptom relief provided by pseudoephedrine in respiratory conditions typically ranges from 4-6 hours for immediate-release formulations and up to 12 hours for extended-release preparations. In bronchitis contexts, this timing may align poorly with the persistent nature of bronchial inflammation, which often requires weeks for complete resolution. Patient-reported outcomes suggest variable responses to pseudoephedrine in bronchitis, with some individuals experiencing meaningful symptom improvement while others derive minimal benefit beyond transient nasal decongestion. The heterogeneous response patterns likely reflect differences in individual pathophysiology, symptom severity, and concurrent upper respiratory involvement among bronchitis patients.
Pharmacokinetic considerations and dosage protocols
The pharmacokinetic profile of pseudoephedrine hydrochloride influences its therapeutic utility in managing bronchitis symptoms and determines optimal dosing strategies for respiratory applications. Understanding absorption patterns, distribution characteristics, and elimination pathways helps clinicians and patients maximise therapeutic benefits while minimising potential adverse effects. The medication’s bioavailability approaches 100% following oral administration, with minimal first-pass hepatic metabolism ensuring consistent systemic exposure across individuals. These pharmacokinetic properties contribute to predictable therapeutic responses but also necessitate careful attention to dosing intervals and total daily exposure limits.
Standard pseudoephedrine dosing regimens for respiratory symptoms
Standard pseudoephedrine dosing for respiratory symptoms involves 60mg every 4-6 hours for immediate-release formulations, with maximum daily doses not exceeding 240mg in healthy adults. Extended-release preparations typically utilise 120mg every 12 hours or 240mg once daily, providing sustained therapeutic levels throughout the dosing interval. Paediatric dosing calculations require weight-based adjustments, with children aged 6-12 years receiving 30mg every 4-6 hours or 4mg/kg/day divided into appropriate intervals. For bronchitis applications, these standard regimens may require modification based on symptom severity and concurrent medication use, particularly when combining with other respiratory therapeutics.
Absorption kinetics and peak plasma concentration timeline
Following oral administration of 60mg pseudoephedrine hydrochloride, peak plasma concentrations of approximately 180-300 ng/mL occur within 1.39-2 hours under fasting conditions. Food intake delays absorption without significantly affecting total bioavailability, suggesting flexible dosing options for patients with varying meal schedules. The rapid absorption profile enables relatively quick symptom onset, with decongestant effects typically beginning within 30 minutes of administration. Extended-release formulations demonstrate delayed peak concentrations occurring 3.8-6.1 hours post-dose, providing more sustained therapeutic levels suitable for nighttime dosing or patients requiring prolonged symptom control.
Hepatic metabolism through CYP2D6 enzyme pathway
Pseudoephedrine undergoes minimal hepatic metabolism, with less than 1% of administered doses undergoing N-demethylation to inactive metabolites. The majority of the drug (55-96%) is excreted unchanged in urine, making renal function the primary determinant of elimination rates rather than hepatic enzyme activity. This metabolic pattern reduces the risk of significant drug-drug interactions compared to medications requiring extensive hepatic biotransformation. However, urinary pH significantly influences elimination kinetics, with acidic urine (pH 5) accelerating excretion and alkaline urine (pH 8) prolonging half-life from 3-6 hours to 9-16 hours respectively.
Contraindications in hypertension and cardiac conditions
Pseudoephedrine carries significant contraindications for patients with severe uncontrolled hypertension, coronary artery disease, and cardiac arrhythmias due to its sympathomimetic properties. The medication can increase blood pressure, heart rate, and myocardial oxygen demand, potentially precipitating cardiovascular events in susceptible individuals. Absolute contraindications include severe coronary artery disease, uncontrolled hypertension, and concurrent monoamine oxidase inhibitor therapy, which can result in hypertensive crisis. Patients with diabetes, hyperthyroidism, or prostatic hyperplasia require careful monitoring and dose adjustments to prevent exacerbation of underlying conditions while managing bronchitis symptoms.
Alternative bronchitis treatment modalities and comparative analysis
While pseudoephedrine may provide symptomatic relief for certain aspects of bronchitis, multiple alternative therapeutic approaches offer more targeted treatment of the underlying pathophysiology and associated symptoms. These alternatives range from expectorants designed to enhance mucus clearance to bronchodilators that directly address airway constriction. Comprehensive bronchitis management often incorporates multiple therapeutic modalities to address the diverse symptom complex, including persistent cough, mucus hypersecretion, and respiratory discomfort. Understanding the comparative efficacy and mechanisms of these alternatives helps patients and healthcare providers develop optimal treatment strategies tailored to individual symptom patterns and disease severity.
Guaifenesin expectorant therapy for mucus clearance
Guaifenesin represents the most widely used expectorant for bronchitis management, functioning through mechanisms that enhance respiratory tract fluid secretions and reduce mucus viscosity. The medication stimulates vagal gastric irritant receptors, triggering increased respiratory tract secretions that help thin tenacious sputum and facilitate expectoration. Standard dosing involves 400mg every 4 hours with maximum daily doses of 2400mg, providing sustained effects on mucus consistency and clearance. Clinical evidence supporting guaifenesin efficacy in bronchitis remains modest, with some studies demonstrating improved sputum characteristics and reduced cough frequency compared to placebo treatments.
Dextromethorphan antitussive properties in dry cough management
Dextromethorphan offers antitussive effects through central nervous system mechanisms, specifically targeting the cough centre in the medulla oblongata to suppress non-productive cough reflexes. The medication proves most beneficial for bronchitis patients experiencing dry, irritating cough that interferes with sleep or daily activities. Standard adult dosing involves 15-30mg every 4 hours with maximum daily limits of 120mg, providing 4-8 hours of cough suppression per dose. Important considerations include avoiding dextromethorphan in productive cough scenarios where secretion clearance remains essential for recovery, making timing and patient selection crucial for optimal therapeutic outcomes.
Bronchodilator inhalers including salbutamol and ipratropium
Bronchodilator inhalers may provide significant benefits for bronchitis patients experiencing airway constriction or wheezing, though current guidelines do not routinely recommend their use in uncomplicated acute bronchitis. Salbutamol, a short-acting beta-2 agonist, produces rapid bronchial smooth muscle relaxation and can provide relief within minutes of administration. Ipratropium bromide, an anticholinergic bronchodilator, offers complementary mechanisms through muscarinic receptor antagonism and may prove particularly beneficial for patients with concurrent chronic obstructive pulmonary disease. Evidence suggests that bronchodilators provide minimal benefit for otherwise healthy individuals with acute bronchitis, though they may play important roles in patients with underlying respiratory conditions or those experiencing significant airway reactivity.
Drug
interaction profiles and safety considerations
Pseudoephedrine demonstrates significant potential for drug interactions, particularly with medications affecting cardiovascular function and central nervous system activity. The most critical interaction involves monoamine oxidase inhibitors (MAOIs), which can precipitate hypertensive crisis when combined with sympathomimetic agents. This potentially fatal interaction requires a minimum two-week washout period between MAOI discontinuation and pseudoephedrine initiation, with similar precautions applying when transitioning from pseudoephedrine to MAOI therapy. Healthcare providers must carefully screen patients for concurrent medication use, particularly antidepressants, before recommending pseudoephedrine for bronchitis symptom management.
Cardiovascular medications including beta-blockers, ACE inhibitors, and antiarrhythmic drugs may experience reduced efficacy when combined with pseudoephedrine due to opposing pharmacological mechanisms. The sympathomimetic effects of pseudoephedrine can counteract blood pressure reduction achieved through antihypertensive therapy, potentially necessitating dose adjustments or alternative treatment approaches. Patients taking digoxin face increased risk of cardiac arrhythmias when combined with pseudoephedrine, as both medications can increase myocardial irritability and alter cardiac conduction patterns. Regular monitoring becomes essential for patients requiring concurrent therapy with these medication classes.
The combination of pseudoephedrine with other sympathomimetic medications found in cold and flu preparations can lead to additive effects and increased risk of adverse cardiovascular events
particularly in susceptible individuals. This includes phenylephrine-containing nasal decongestants, caffeine from beverages or medications, and stimulant medications used for attention deficit disorders.
Safety considerations extend beyond drug interactions to encompass patient-specific factors that influence pseudoephedrine tolerability and efficacy in bronchitis treatment. Elderly patients demonstrate increased sensitivity to sympathomimetic effects, experiencing higher rates of cardiovascular complications, sleep disturbances, and cognitive effects. Age-related changes in drug metabolism and clearance may necessitate dose reductions or extended dosing intervals to maintain safety while preserving therapeutic benefits. Paediatric safety concerns focus on appropriate dose calculations and avoiding formulations containing multiple active ingredients that could lead to inadvertent overdosing.
Pregnancy and lactation present additional safety considerations, as pseudoephedrine crosses the placental barrier and appears in breast milk at concentrations potentially affecting infant physiology. While current evidence does not definitively establish teratogenic risks, the medication may reduce milk production and cause irritability in nursing infants. Risk-benefit assessments must carefully weigh potential maternal symptom relief against foetal and infant safety concerns, often favouring alternative treatment approaches during these vulnerable periods. Healthcare providers should explore non-pharmacological interventions and safer medication alternatives before considering pseudoephedrine therapy in pregnant or lactating women with bronchitis symptoms.
The pharmacovigilance profile of pseudoephedrine reveals important patterns of adverse effects that influence its appropriateness for bronchitis treatment across different patient populations. Common side effects including insomnia, nervousness, and appetite suppression may compound the fatigue and discomfort already experienced by bronchitis patients. More serious adverse effects such as hypertension, cardiac arrhythmias, and seizures, while rare, underscore the importance of appropriate patient selection and monitoring protocols. These safety considerations help explain why current clinical guidelines emphasise supportive care and symptom-specific treatments over broad-spectrum decongestant therapy for most bronchitis patients, reserving pseudoephedrine for carefully selected cases where benefits clearly outweigh potential risks.