When earache coincides with swollen lymph nodes, particularly those located behind the ear or in the neck region, it often indicates that your body is mounting an immune response against an infectious pathogen. This combination of symptoms represents a complex interplay between localised infection within the ear structures and the regional lymphatic system’s defensive mechanisms. The temporal relationship between otalgia and lymphadenopathy can provide valuable diagnostic insights, helping healthcare professionals distinguish between simple viral infections and more serious bacterial complications that may require immediate antibiotic intervention.
Understanding the anatomical connection between otitis media and cervical lymphadenopathy
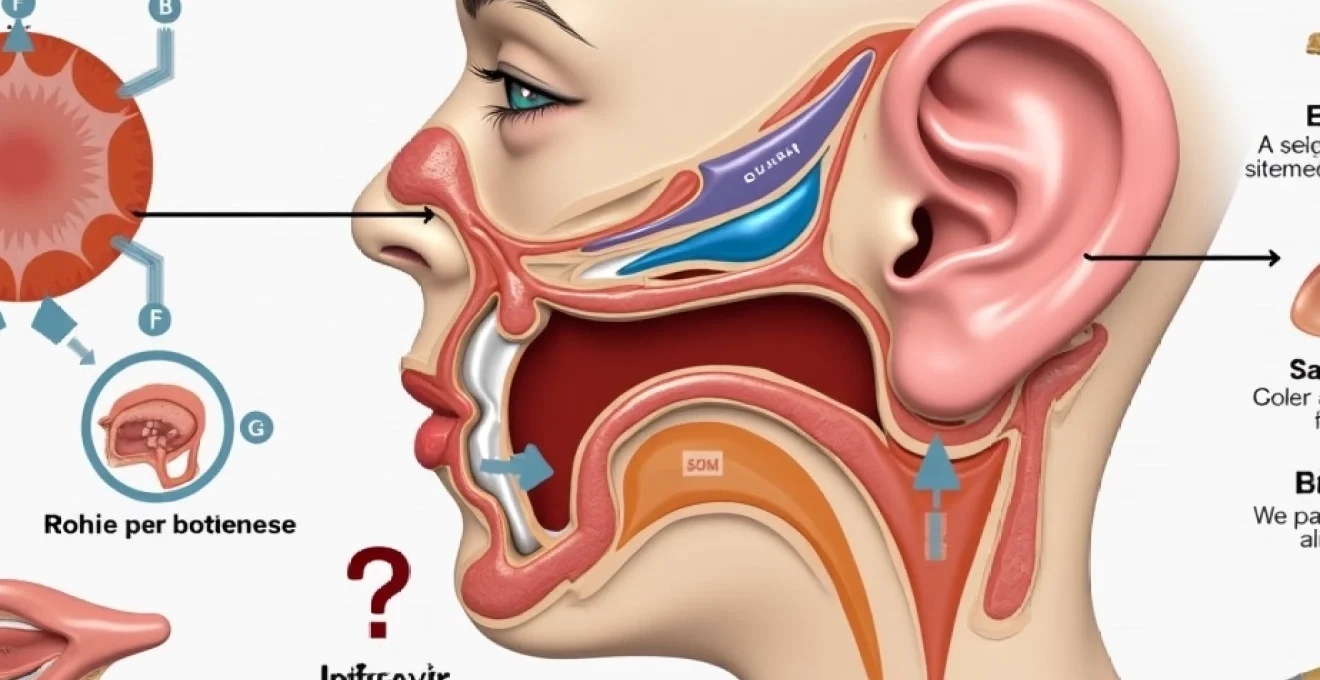
The intricate relationship between ear infections and lymph node enlargement stems from the sophisticated lymphatic drainage network surrounding the temporal bone and middle ear cavity. When pathogens invade the middle ear space, they trigger a cascade of inflammatory responses that extend far beyond the confines of the tympanic cavity itself. The anatomical positioning of various lymph node groups creates distinct drainage patterns that can help clinicians localise the source of infection based on which specific nodes become enlarged.
Eustachian tube dysfunction and secondary lymphatic drainage patterns
Eustachian tube dysfunction creates a unique environment that predisposes individuals to both middle ear infections and subsequent lymphatic involvement. When the eustachian tube fails to equalise pressure effectively, fluid accumulation occurs within the middle ear space, providing an ideal breeding ground for bacterial proliferation. This stagnant environment allows pathogens to multiply unchecked, eventually overwhelming local immune defences and triggering regional lymph node activation. The inflammatory mediators released during this process travel through lymphatic channels, causing characteristic swelling in preauricular, postauricular, and upper cervical node groups.
Middle ear inflammatory response triggering regional node activation
The middle ear’s inflammatory response involves a complex network of cytokines and chemokines that directly influence lymphatic vessel permeability and lymph node function. When bacterial toxins or viral particles penetrate the middle ear mucosa, they activate local immune cells, including macrophages and dendritic cells, which subsequently migrate to regional lymph nodes. This migration process carries infectious material and inflammatory signals to the lymphatic system, where specialised immune cells work to contain and eliminate the threat. The resulting lymph node enlargement serves as both a defensive mechanism and a visible indicator of ongoing infection.
Pathophysiology of retroauricular and submandibular lymph node enlargement
Retroauricular lymph nodes, positioned behind the ear along the posterior edge of the sternocleidomastoid muscle, serve as primary drainage sites for infections affecting the external auditory canal and mastoid air cells. These nodes typically measure less than one centimetre in healthy individuals but can expand significantly during active infections. Submandibular lymph nodes, located beneath the jaw line, often become involved when middle ear infections spread to involve the throat or when concurrent upper respiratory tract infections occur. The pattern of node involvement can provide valuable clues about the extent and progression of the underlying infectious process.
Temporal bone infection spread via lymphatic vessels
Temporal bone infections represent a particularly concerning scenario where the lymphatic spread pattern can indicate potential complications such as mastoiditis or intracranial extension. The temporal bone contains numerous air cells that communicate with the middle ear space, and infections can track through these interconnected chambers via lymphatic pathways. When infections spread beyond the middle ear to involve mastoid air cells, the resulting inflammatory response often produces pronounced swelling in posterior cervical and occipital lymph node groups. This pattern of lymphadenopathy should prompt immediate evaluation for potential surgical intervention to prevent serious complications.
Primary infectious aetiologies causing concurrent otalgia and lymphadenitis
The spectrum of infectious organisms responsible for combined ear pain and lymph node swelling encompasses both bacterial and viral pathogens, each producing characteristic clinical patterns that can guide diagnostic and therapeutic decisions. Understanding these distinct presentations enables healthcare providers to implement appropriate treatment strategies while monitoring for potential complications. The temporal progression of symptoms, combined with specific lymph node involvement patterns, often provides crucial information about the likely causative organism and expected disease course.
Streptococcus pneumoniae-induced acute otitis media with nodal response
Streptococcus pneumoniae remains one of the most common bacterial causes of acute otitis media, particularly in paediatric populations where eustachian tube anatomy predisposes to infection. This organism produces potent inflammatory responses that typically result in rapid onset of severe ear pain accompanied by fever and malaise. The pneumococcal inflammatory response characteristically triggers enlargement of preauricular and upper cervical lymph nodes within 24-48 hours of symptom onset. These infections often respond well to appropriate antibiotic therapy, with lymph node swelling typically resolving within one to two weeks following successful treatment.
Haemophilus influenzae bacterial colonisation and lymphatic involvement
Haemophilus influenzae, particularly non-typeable strains, frequently colonises the upper respiratory tract and can ascend through the eustachian tube to cause middle ear infections. This organism has a particular affinity for mucus-producing surfaces and can establish biofilm formations that make infections particularly persistent and difficult to eradicate. The lymphatic response to H. influenzae infections tends to be more gradual than that seen with pneumococcal infections, with lymph nodes enlarging progressively over several days. These infections may require extended antibiotic courses and careful monitoring to ensure complete resolution.
Viral upper respiratory tract infections: rhinovirus and adenovirus patterns
Viral upper respiratory tract infections frequently precede and predispose to secondary bacterial otitis media, creating a complex clinical picture that combines viral and bacterial inflammatory responses. Rhinovirus infections typically cause eustachian tube dysfunction through mucosal swelling and increased secretions, creating conditions favourable for bacterial superinfection. Adenovirus infections can produce more severe inflammatory responses, sometimes mimicking bacterial infections in their clinical presentation. The lymphatic response to viral infections tends to be more generalised, often involving multiple node groups bilaterally rather than the focal enlargement typically seen with bacterial processes.
Moraxella catarrhalis biofilm formation in chronic suppurative cases
Moraxella catarrhalis has emerged as an increasingly important pathogen in chronic suppurative otitis media, particularly in cases involving persistent drainage and recurrent symptoms. This organism’s ability to form complex biofilms within the middle ear space makes infections particularly challenging to treat and prone to recurrence. The chronic inflammatory response associated with M. catarrhalis infections often produces persistent lymph node enlargement that may persist for weeks or months despite appropriate antibiotic therapy. These cases frequently require comprehensive evaluation including culture-directed antibiotic selection and consideration of surgical intervention for definitive management.
Differential diagnosis of malignant versus reactive lymphadenopathy in ear conditions
Distinguishing between reactive lymphadenopathy secondary to infectious processes and malignant lymph node involvement requires careful consideration of multiple clinical factors, including patient age, symptom duration, node characteristics, and associated systemic symptoms. While the vast majority of lymph node enlargement in the setting of ear pain represents benign reactive changes, certain clinical features should prompt more extensive evaluation to exclude malignant processes. The presence of constitutional symptoms such as unexplained weight loss, night sweats, or persistent fever may indicate underlying malignancy requiring urgent investigation.
Lymph nodes that remain enlarged for more than six weeks following resolution of acute infection, measure greater than two centimetres in diameter, or feel firm and immobile on palpation warrant immediate specialist evaluation and potential biopsy.
Reactive lymphadenopathy typically presents with tender, mobile nodes that enlarge rapidly during acute infection and gradually resolve over several weeks as the underlying infection clears. These nodes usually maintain a soft, rubbery consistency and may be slightly warm to touch during active inflammation. In contrast, malignant lymph nodes tend to be painless, firm or hard in consistency, and may feel fixed to surrounding tissues. The pattern of involvement also differs significantly, with malignant processes often affecting multiple node groups simultaneously or in a predictable anatomical progression.
Age represents a crucial factor in the differential diagnosis, as lymphomas and other malignant processes become increasingly common in older adults, while reactive lymphadenopathy predominates in younger patients. However, certain malignancies, including acute lymphoblastic leukaemia, can present with lymphadenopathy in paediatric populations, making thorough evaluation essential regardless of patient age. The temporal relationship between ear symptoms and lymph node enlargement also provides important diagnostic information, with synchronous development suggesting reactive changes while lymphadenopathy preceding ear symptoms may indicate malignant involvement.
Clinical assessment techniques for otolaryngological lymphatic examination
Comprehensive assessment of patients presenting with concurrent ear pain and lymphadenopathy requires systematic examination techniques that evaluate both the primary site of infection and the regional lymphatic response. The physical examination should follow a standardised approach that includes inspection, palpation, and documentation of lymph node characteristics, combined with detailed otoscopic examination to identify the source and severity of ear pathology. Proper examination technique is essential for accurate diagnosis and appropriate treatment planning.
Palpation methodology for preauricular and postauricular node groups
Systematic palpation of lymph nodes requires a methodical approach using the fingertips rather than the thumb, applying gentle circular motions to assess node size, consistency, mobility, and tenderness. Begin the examination with the patient seated comfortably, head slightly tilted away from the examiner to relax the neck muscles. Preauricular nodes are best palpated just anterior to the tragus, using light pressure to avoid discomfort while ensuring adequate assessment of deeper structures. The examination should progress systematically from preauricular to postauricular nodes, located behind the ear along the mastoid process, then continue down the neck to assess submandibular, submental, and cervical chain nodes.
Otoscopic findings correlating with specific lymphatic drainage zones
Otoscopic examination findings can provide valuable information about which lymph node groups are likely to be affected based on the anatomical drainage patterns of different ear structures. Acute otitis media with tympanic membrane erythema and bulging typically correlates with preauricular and upper cervical node enlargement, reflecting the primary drainage pathway from the middle ear space. External otitis affecting the ear canal often produces postauricular lymphadenopathy due to the drainage pattern from the external auditory canal. Chronic otitis media with perforation and drainage may involve multiple node groups, reflecting the complex inflammatory response and potential for ascending infection.
Weber and rinne test interpretations in lymphadenopathic presentations
Tuning fork tests provide valuable information about the type and degree of hearing loss associated with ear infections and can help correlate clinical findings with lymphatic involvement patterns. The Weber test, performed by placing a vibrating tuning fork on the patient’s forehead or vertex, typically lateralises to the affected ear in cases of conductive hearing loss secondary to middle ear infection. The Rinne test compares air and bone conduction, with bone conduction exceeding air conduction indicating conductive hearing loss consistent with middle ear pathology. These findings, combined with lymph node assessment, help confirm the diagnosis of middle ear infection and guide appropriate treatment decisions.
Diagnostic imaging protocols: CT versus MRI for complicated otitis cases
Advanced imaging studies become essential when clinical findings suggest complicated ear infections or when lymphadenopathy patterns raise concern for serious underlying pathology. The choice between computed tomography and magnetic resonance imaging depends on the specific clinical scenario, with each modality offering distinct advantages for evaluating different aspects of ear and lymph node pathology. Understanding the appropriate applications of each imaging technique ensures optimal diagnostic accuracy while minimising unnecessary radiation exposure and healthcare costs.
Computed tomography with contrast enhancement provides excellent visualisation of temporal bone anatomy and is particularly valuable for assessing mastoid air cell involvement, bone erosion, and potential intracranial complications. CT imaging excels at detecting mastoiditis , cholesteatoma, and other structural complications that may require surgical intervention. The ability to perform rapid acquisition makes CT ideal for emergency situations where prompt diagnosis is essential for preventing serious complications. However, CT provides limited soft tissue contrast resolution and exposes patients to ionising radiation, making it less suitable for repeated follow-up examinations.
MRI offers superior soft tissue contrast resolution and is particularly valuable for evaluating lymph node characteristics, distinguishing between reactive and malignant enlargement, and assessing potential intracranial extension of infection.
Magnetic resonance imaging provides detailed information about lymph node internal architecture, helping differentiate between reactive hyperplasia and malignant infiltration based on signal characteristics and enhancement patterns. MRI can identify early signs of complications such as sigmoid sinus thrombosis, epidural abscess, or brain parenchymal involvement that may not be apparent on CT imaging. The multiplanar capabilities of MRI allow comprehensive evaluation of the relationship between infected structures and surrounding anatomy, facilitating surgical planning when intervention is required. However, MRI examinations take significantly longer to perform and may require sedation in paediatric patients or those with claustrophobia.
The decision between CT and MRI should consider patient age, clinical presentation severity, suspected complications, and the need for urgent intervention. Emergency situations with suspected intracranial complications typically warrant immediate CT evaluation, while chronic or recurrent cases with atypical lymphadenopathy may benefit from MRI assessment. In some complex cases, both imaging modalities may be necessary to provide comprehensive evaluation of all relevant anatomical structures and pathological processes.
Evidence-based treatment algorithms for Antibiotic-Responsive Ear-Node syndromes
Contemporary management of ear infections with associated lymphadenopathy requires evidence-based antibiotic selection that considers local resistance patterns, patient-specific factors, and the severity of clinical presentation. Treatment algorithms must balance the need for effective antimicrobial therapy against the growing concern for antibiotic resistance and adverse effects. The approach to antibiotic selection should consider the most likely causative organisms based on patient age, clinical presentation, and epidemiological factors specific to the geographic region.
First-line antibiotic therapy for uncomplicated acute otitis media with lymphadenopathy typically involves high-dose amoxicillin, which remains effective against most strains of Streptococcus pneumoniae and provides good middle ear penetration. The recommended dosage is 80-90 mg/kg/day divided into two or three doses for paediatric patients, with adult dosing typically ranging from 1000-1500mg twice daily. This approach provides adequate coverage for the most common bacterial pathogens while maintaining a favourable safety profile and relatively low cost. Treatment duration should typically extend for 10-14 days to ensure complete bacterial eradication and prevent recurrence.
Patients with penicillin allergies or those living in areas with high rates of beta-lactamase producing organisms may require alternative antibiotic regimens such as azithromycin, clarithromycin, or ceftriaxone. Azithromycin offers the advantage of shorter treatment courses and excellent tissue penetration, making it particularly useful for patients with compliance concerns. However, increasing macrolide resistance among pneumococcal isolates necessitates careful consideration of local resistance patterns when selecting this option. Fluoroquinolone antibiotics such as ciprofloxacin may be necessary for cases involving Pseudomonas aeruginosa or other gram-negative organisms, particularly in the setting of chronic otitis media with perforation.
Treatment failure, defined as persistence or worsening of symptoms after 48-72 hours of appropriate antibiotic therapy, requires reassessment of the diagnosis and consideration of alternative antimicrobial regimens. Factors contributing to treatment failure include antibiotic resistance, inadequate dosing, poor compliance, or the presence of complications such as mastoiditis or intracranial extension. In such cases, culture and sensitivity testing should be obtained when possible, and empirical therapy should be broadened to cover resistant organisms. Patients with treatment failure may require parenteral antibiotic administration or surgical intervention to achieve clinical resolution.
Follow-up protocols should include clinical reassessment at regular intervals to monitor treatment response and lymph node resolution. Most patients experience significant symptomatic improvement within 48-72 hours of initiating appropriate antibiotic therapy, with complete resolution expected within 7-10 days. Lymph node swelling typically begins to decrease within the first week of treatment but may persist for several weeks after clinical resolution of the ear infection. Patients should be advised to complete the entire antibiotic course even if symptoms improve rapidly, as premature discontinuation increases the risk of treatment failure and bacterial resistance development.