Pelvic misalignment affects a staggering 8 out of 10 individuals, making it one of the most prevalent yet underdiagnosed musculoskeletal conditions. Research indicates that approximately 85% of males and 75% of females present with some degree of pelvic asymmetry, particularly anterior pelvic tilt. This seemingly subtle structural deviation can trigger a cascade of compensatory mechanisms throughout the kinetic chain, leading to chronic pain patterns that extend far beyond the pelvis itself.
The complexity of pelvic anatomy means that even minor misalignments can significantly impact your daily functioning. Your pelvis serves as the central foundation connecting your spine to your lower extremities, orchestrating movement patterns and weight distribution. When this crucial junction becomes compromised, the resulting symptoms often manifest in unexpected locations, from persistent lower back pain to seemingly unrelated issues such as neck tension or even dental problems from teeth grinding.
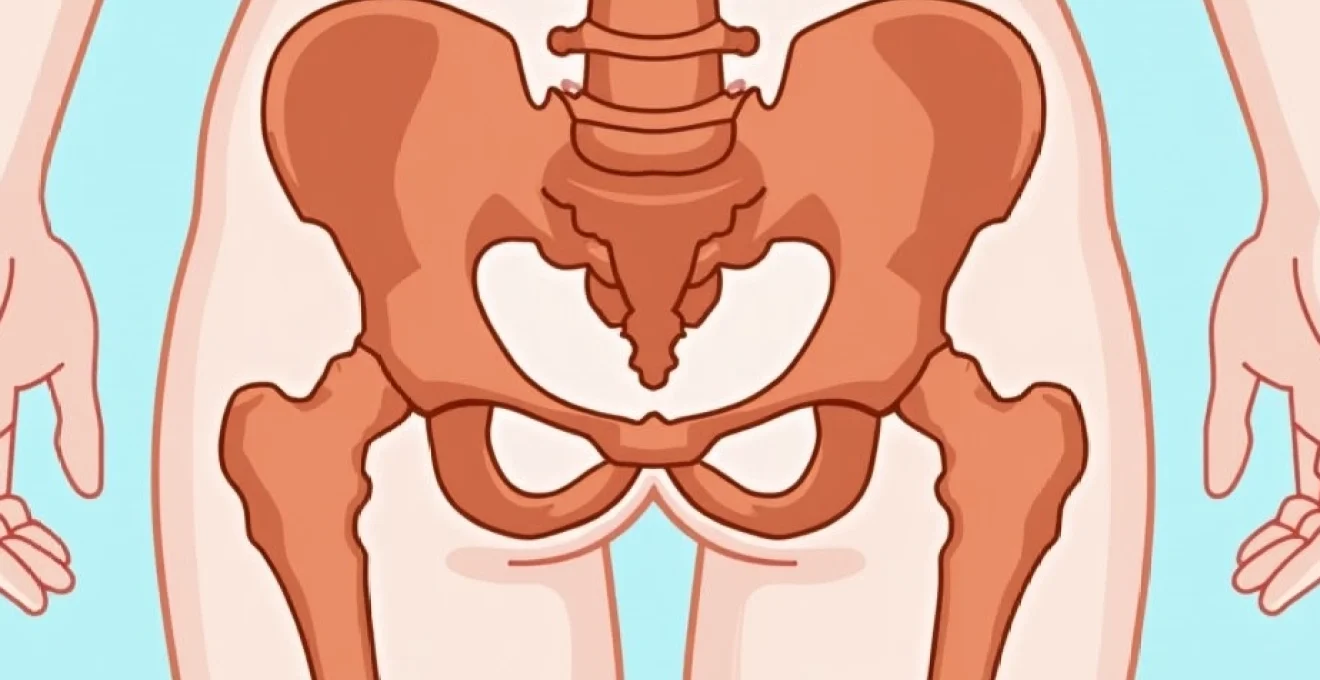
Anatomical structure of pelvic alignment and biomechanical function
The pelvic girdle comprises three primary bones: the paired iliac bones and the sacrum, which collectively form a rigid ring structure. This anatomical framework provides stability whilst maintaining flexibility essential for locomotion and weight-bearing activities. The pelvis functions as a sophisticated mechanical system where forces from the upper body transmit through to the lower extremities during movement and static postures.
Understanding proper pelvic alignment requires examining the relationship between key anatomical landmarks. In neutral position, the anterior superior iliac spines (ASIS) should align vertically with the pubic symphysis when viewed from the side. The iliac crests must maintain horizontal symmetry, and the sacroiliac joints should demonstrate equal mobility patterns. This optimal configuration ensures efficient force transmission and minimises compensatory stress patterns throughout the musculoskeletal system.
Sacroiliac joint dysfunction and positional asymmetry
The sacroiliac joints represent critical articulations where the sacrum meets the iliac bones, forming the posterior aspect of the pelvic ring. These joints possess limited mobility but play crucial roles in shock absorption and load transfer between the spine and lower extremities. When sacroiliac joint dysfunction occurs, asymmetrical movement patterns develop, creating rotational stress throughout the pelvic complex.
Positional asymmetry at the sacroiliac joints often manifests as unilateral restrictions in joint mobility. You might experience this as a sensation of “locking” on one side of your lower back, particularly when transitioning from sitting to standing positions. The resulting compensatory patterns can trigger muscle guarding responses in the gluteal region and deep hip rotators, perpetuating the cycle of dysfunction.
Anterior and posterior pelvic tilt mechanisms
Anterior pelvic tilt represents the most common form of pelvic misalignment, characterised by forward rotation of the pelvis around a horizontal axis. This positioning increases lumbar lordosis and creates excessive lengthening of the posterior chain muscles whilst shortening hip flexors and lumbar extensors. The resulting postural deviation places abnormal stress on the lumbar facet joints and intervertebral discs.
Posterior pelvic tilt, whilst less prevalent, involves backward rotation of the pelvis, flattening the natural lumbar curve. This configuration often accompanies thoracic kyphosis and forward head posture, creating a characteristic slouched appearance. The biomechanical consequences include increased pressure on anterior disc structures and reduced shock-absorbing capacity of the spinal curves.
Iliac crest height discrepancies and lateral pelvic shift
Lateral pelvic asymmetries manifest as differences in iliac crest heights, creating functional or structural leg length discrepancies. These imbalances force the spine into compensatory scoliotic curves to maintain visual horizontal alignment. The resulting postural adaptations can trigger complex pain patterns extending from the feet to the cervical spine.
Functional leg length discrepancies often result from muscle imbalances and postural habits rather than actual bone length differences. Chronic unilateral weight-bearing, occupational postures, or repetitive movement patterns can create adaptive shortening in specific muscle groups, pulling one side of the pelvis higher than the other. This type of asymmetry typically responds well to conservative interventions targeting muscle balance restoration.
Pubic symphysis separation and rotational malalignment
The pubic symphysis forms the anterior junction of the pelvic ring, maintaining stability through a fibrocartilaginous disc and strong ligamentous attachments. Separation or malalignment at this joint commonly occurs during pregnancy and childbirth but can also result from trauma or repetitive stress activities. Pubic symphysis dysfunction creates characteristic groin pain and difficulty with weight-bearing activities.
Rotational malalignment patterns involve asymmetrical positioning of the innominate bones relative to the sacrum. These complex three-dimensional deviations can create anterior rotation on one side whilst the contralateral side rotates posteriorly. The resulting mechanical dysfunction affects hip joint biomechanics and creates compensatory movement patterns throughout the lower extremity kinetic chain.
Clinical symptomatology of pelvic misalignment patterns
Pelvic misalignment presents through diverse symptom patterns that can confound both patients and healthcare providers. The interconnected nature of the musculoskeletal system means that pelvic dysfunction rarely remains localised, instead creating referral patterns that can manifest throughout the body. Understanding these symptom presentations is crucial for accurate diagnosis and effective treatment planning.
The onset of symptoms associated with pelvic misalignment typically follows a gradual progression, beginning with subtle discomfort that may be dismissed as normal aging or activity-related soreness. However, as compensatory patterns become established, symptom intensity and frequency increase, often reaching a point where daily activities become significantly impacted. The key to successful management lies in recognising these early warning signs before chronic adaptations become entrenched.
Lower back pain radiating through L4-L5 vertebral segments
Lower back pain represents the most common presenting complaint in individuals with pelvic misalignment. The pain typically localises to the L4-L5 and L5-S1 segments, corresponding to areas of maximum mechanical stress created by altered pelvic positioning. This discomfort often intensifies with prolonged sitting or standing, reflecting the increased load on these spinal segments during static postures.
The radiating component of lower back pain frequently follows dermatomal patterns consistent with nerve root irritation. You might experience shooting pains extending into the posterior thigh or lateral leg, accompanied by numbness or tingling sensations. These neurological symptoms indicate compression or irritation of spinal nerve roots as they exit the neural foramina, often exacerbated by inflammatory responses to chronic mechanical stress.
Hip flexor contracture and piriformis syndrome manifestations
Hip flexor contracture commonly develops as a consequence of anterior pelvic tilt, creating characteristic symptoms of anterior hip pain and restricted hip extension. The iliopsoas muscle group becomes adaptively shortened, limiting your ability to achieve full hip extension during walking or running activities. This restriction forces compensatory movement patterns that can trigger secondary problems in the knee and ankle joints.
Piriformis syndrome frequently accompanies lateral pelvic asymmetries, as the deep hip rotator muscles attempt to compensate for altered hip joint mechanics. The piriformis muscle can become hypertrophic and irritated, potentially compressing the sciatic nerve as it passes through or adjacent to the muscle belly. This condition creates deep buttock pain that may radiate down the posterior leg, often mistaken for disc-related sciatica.
Sciatica and neurological compression symptoms
True sciatica resulting from pelvic misalignment occurs when altered spinal mechanics create compression of the sciatic nerve roots at the L4-S3 levels. The characteristic burning or electric shock-like pain follows the sciatic nerve distribution, extending from the lower back through the buttock and down the posterior or lateral leg. Coughing, sneezing, or straining activities typically exacerbate these symptoms by increasing intraspinal pressure.
Neurological compression symptoms may also include motor weakness in specific muscle groups innervated by affected nerve roots. You might notice difficulty with toe walking (S1 nerve root) or heel walking (L5 nerve root), indicating more severe compression requiring prompt medical attention. Bladder or bowel dysfunction represents a medical emergency and necessitates immediate evaluation to rule out cauda equina syndrome.
Compensatory gait abnormalities and postural deviations
Pelvic misalignment inevitably affects gait patterns as your body attempts to maintain balance and forward progression despite structural asymmetries. Common gait deviations include Trendelenburg patterns, where the pelvis drops on the non-weight-bearing side due to gluteus medius weakness, and antalgic gait patterns characterised by shortened stance phases on the affected side to minimise pain.
Postural deviations extend beyond the pelvis to encompass the entire axial skeleton. Forward head posture often accompanies anterior pelvic tilt as the cervical spine extends to maintain visual horizontal orientation. Shoulder asymmetries may develop, with one shoulder elevated relative to the other, creating potential for secondary neck and shoulder pain syndromes. These compensatory patterns can become so ingrained that they persist even after primary pelvic dysfunction resolves.
Diagnostic assessment methods for pelvic malalignment
Accurate diagnosis of pelvic misalignment requires systematic evaluation combining clinical observation, functional testing, and imaging studies when appropriate. The complexity of pelvic dysfunction necessitates a comprehensive approach that considers both structural and functional components of the presentation. Modern diagnostic protocols emphasise the importance of dynamic assessment methods that evaluate movement patterns rather than relying solely on static postural observations.
Clinical assessment begins with detailed history-taking to identify potential contributing factors such as occupational demands, recreational activities, previous injuries, or pregnancy-related changes. The temporal relationship between symptom onset and specific activities or life events often provides valuable diagnostic clues. Understanding the patient’s pain patterns, including aggravating and alleviating factors, helps differentiate between various causes of pelvic dysfunction.
Standing forward bend test and seated flexion examination
The standing forward bend test, also known as the Adam’s forward bend test, provides valuable information about spinal alignment and pelvic symmetry during functional movement. During this examination, you bend forward from the waist whilst the examiner observes from behind, noting any asymmetries in rib prominence, spinal curvature, or pelvic positioning. Significant asymmetries may indicate structural scoliosis or functional imbalances requiring further investigation.
The seated flexion examination isolates hip and pelvic motion by eliminating the influence of leg length discrepancies. This test involves forward flexion whilst seated, allowing assessment of sacroiliac joint mobility and detecting restrictions or asymmetries in movement patterns. Positive findings suggest sacroiliac joint dysfunction or myofascial restrictions affecting pelvic mechanics.
Gillet test for sacroiliac joint mobility assessment
The Gillet test, or one-legged stork test, evaluates sacroiliac joint mobility by assessing the movement relationship between the sacrum and ilium during hip flexion. The examiner palpates the posterior superior iliac spine and median sacral crest whilst you flex one hip toward the chest. Normal findings show inferior movement of the PSIS relative to the sacrum, indicating proper sacroiliac joint mobility.
Positive Gillet test results suggest sacroiliac joint restriction or hypomobility on the tested side. This finding, combined with pain provocation during the manoeuvre, strongly indicates sacroiliac joint dysfunction as a contributing factor to your symptoms. The test’s specificity improves when combined with other provocation tests such as the compression and distraction tests.
Radiographic analysis using ferguson’s view and AP pelvis imaging
Ferguson’s view radiography provides specific visualisation of the lumbosacral junction and sacroiliac joints by angling the X-ray beam 30-35 degrees caudally. This projection optimises visualisation of L5-S1 disc space narrowing, spondylolisthesis, and sacroiliac joint abnormalities that may contribute to pelvic dysfunction. The technique proves particularly valuable in detecting subtle structural abnormalities not visible on standard AP and lateral views.
Anteroposterior pelvis radiographs allow measurement of various pelvic parameters including acetabular coverage, hip joint spacing, and overall pelvic symmetry. Digital analysis can quantify leg length discrepancies and measure pelvic obliquity with high precision. These measurements guide treatment planning and help differentiate between structural and functional causes of pelvic asymmetry.
Functional leg length discrepancy measurement techniques
Functional leg length assessment involves multiple measurement techniques to differentiate between true anatomical discrepancies and apparent differences caused by pelvic positioning. The supine-to-sit test evaluates changes in apparent leg length between lying and sitting positions, helping identify sacroiliac joint dysfunction patterns. Significant changes in relative leg lengths between positions suggest functional rather than structural discrepancies.
Tape measure assessments from the anterior superior iliac spine to the medial malleolus provide quantitative data regarding apparent leg length differences. However, pelvic positioning significantly influences these measurements, necessitating careful standardisation of patient positioning. Block tests, where graduated blocks are placed under the shorter leg until pelvic leveling occurs, offer practical information for orthotic prescription and treatment planning.
Musculoskeletal pain distribution in pelvic asymmetry
The pain patterns associated with pelvic asymmetry follow predictable anatomical pathways that reflect the interconnected nature of the musculoskeletal system. Understanding these distribution patterns enables more accurate diagnosis and targeted treatment approaches. Pain rarely remains confined to the pelvis itself, instead manifesting through complex referral patterns that can extend from the cervical spine to the feet.
Myofascial trigger points commonly develop in muscles attempting to compensate for pelvic misalignment, creating characteristic referred pain patterns. The gluteus medius frequently develops trigger points that refer pain to the posterior hip and lateral thigh, whilst quadratus lumborum trigger points create deep aching sensations in the lower back and buttock regions. These referral patterns often confuse the clinical picture, as the site of pain may be distant from the actual source of dysfunction.
Visceral pain patterns can also be influenced by pelvic misalignment through alteration of autonomic nervous system function. Chronic pelvic dysfunction may affect sacral nerve root function, potentially influencing bladder, bowel, and reproductive organ innervation. Women with pelvic misalignment may experience menstrual irregularities or pelvic floor dysfunction, whilst men might report changes in urinary function or sexual performance.
The central nervous system’s adaptation to chronic pelvic misalignment can create persistent pain patterns that continue even after structural corrections are achieved, highlighting the importance of comprehensive treatment approaches that address both mechanical and neurological components.
Joint-related pain patterns typically follow biomechanical stress distributions created by altered weight-bearing patterns. The contralateral hip joint often experiences increased loading in cases of unilateral pelvic elevation, potentially accelerating degenerative changes and creating secondary osteoarthritic symptoms. Similarly, compensatory spinal curvatures can overload facet joints at specific spinal levels, creating regional pain and stiffness patterns.
Nerve entrapment syndromes commonly accompany pelvic misalignment as altered anatomy creates compression points along peripheral nerve pathways. The lateral femoral cutaneous nerve may become entrapped as it passes near the anterior superior iliac spine, creating meralgia paresthetica with characteristic numbness and burning sensations along the lateral thigh. These nerve-related symptoms often respond dramatically to correction of underlying pelvic positioning.
Conservative treatment protocols for pelvic realignment
Conservative management of pelvic misalignment emphasises restoration of optimal biomechanical function through targeted interventions addressing both structural and functional components of the condition. Treatment protocols must be individualised based on specific assessment findings, symptom presentation, and patient lifestyle factors. The most successful approaches combine manual therapy techniques, therapeutic exercise prescription, and patient education to achieve sustainable improvements.
Manual therapy interventions form the cornerstone of conservative pelvic realignment treatment, utilising techniques such as high-velocity low-amplitude manipulations, muscle energy techniques, and myofascial release procedures. Osteopathic and chiropractic approaches focus on restoring normal joint mobility and reducing muscle tension through hands-on techniques. These interventions provide immediate symptomatic relief whilst creating optimal conditions for corrective exercise progression.
Therapeutic exercise prescription must address both mobility restrictions and stability def
icits common in individuals with pelvic dysfunction. Core stabilisation exercises targeting the deep abdominal muscles, pelvic floor, and multifidus provide the foundation for long-term stability. Progressive strengthening programmes must address muscle imbalances, particularly focusing on hip flexor lengthening, gluteal strengthening, and postural muscle reactivation.
Corrective exercise protocols typically begin with gentle mobility work to address restriction patterns identified during assessment. Hip flexor stretching techniques, including the Thomas stretch and lunge variations, help restore normal hip extension range of motion. Piriformis stretching and neural mobilisation exercises address sciatic nerve compression symptoms whilst improving deep hip rotator flexibility.
Postural re-education represents a critical component of conservative treatment, focusing on awareness training and movement pattern correction. Patients learn to recognise and modify habitual postures that perpetuate pelvic misalignment, particularly addressing prolonged sitting positions and occupational ergonomics. Visual feedback using mirrors or postural apps can enhance proprioceptive awareness and facilitate sustainable postural improvements.
Modalities such as heat therapy, ultrasound, and electrical stimulation may provide symptomatic relief whilst supporting the healing process. However, these passive interventions should complement rather than replace active treatment approaches. The evidence strongly supports active participation in corrective exercise programmes over reliance on passive treatment modalities alone.
Research demonstrates that combined manual therapy and exercise interventions achieve superior outcomes compared to either approach used in isolation, with improvement rates exceeding 80% in appropriately selected patients.
Pain management strategies must address both peripheral and central sensitisation components that commonly develop with chronic pelvic dysfunction. Graduated exposure to previously painful activities helps desensitise the nervous system whilst building confidence in movement. Cognitive behavioural approaches addressing pain catastrophising and movement avoidance behaviours significantly enhance treatment outcomes in chronic cases.
Preventive strategies and ergonomic modifications for pelvic stability
Prevention of pelvic misalignment requires a proactive approach that addresses modifiable risk factors before dysfunction develops. The sedentary nature of modern lifestyles creates numerous challenges for maintaining optimal pelvic alignment, making preventive strategies increasingly important for population health. Understanding these risk factors enables individuals to make informed decisions about activity choices and lifestyle modifications that support long-term pelvic stability.
Ergonomic modifications in occupational settings represent perhaps the most impactful preventive intervention available. Prolonged sitting in poorly designed workstations creates the perfect storm for developing anterior pelvic tilt and associated muscle imbalances. Adjustable standing desks, ergonomic seating with proper lumbar support, and regular movement breaks can significantly reduce the risk of developing pelvic dysfunction. The key lies in avoiding static postures for extended periods whilst maintaining neutral spinal alignment during necessary sitting activities.
Exercise prescription for prevention differs significantly from therapeutic protocols, focusing on maintenance of muscle balance and joint mobility rather than correction of existing dysfunctions. Regular participation in activities that promote hip flexor flexibility, such as yoga or Pilates, helps counter the effects of prolonged sitting. Strengthening exercises targeting the posterior chain muscles, including the glutes and hamstrings, provide essential support for maintaining neutral pelvic positioning during daily activities.
Sleep ergonomics play an underappreciated role in pelvic health, as prolonged bed rest in poor positions can perpetuate muscle imbalances developed during waking hours. Side sleeping with appropriate pillow support between the knees maintains neutral hip alignment, whilst stomach sleeping should be avoided due to its tendency to promote lumbar extension and hip flexor shortening. The quality of your mattress and pillow support system directly influences spinal alignment during the eight hours spent sleeping each night.
Footwear choices significantly impact pelvic alignment through their influence on lower extremity biomechanics. High-heeled shoes alter the body’s centre of gravity, forcing compensatory anterior pelvic tilt to maintain balance. Even modest heel heights can create cumulative stress patterns over time, making flat, supportive footwear preferable for daily wear. Custom orthotics may be beneficial for individuals with structural leg length discrepancies or significant foot abnormalities affecting pelvic alignment.
Activity modification strategies focus on identifying and modifying movement patterns that place excessive stress on pelvic structures. Athletes participating in sports requiring repetitive hip flexion or rotation, such as cycling or golf, benefit from sport-specific flexibility and strengthening programmes. Understanding proper lifting techniques and body mechanics reduces the risk of acute pelvic injuries that can lead to chronic dysfunction patterns.
Environmental modifications in the home and workplace can support healthy movement patterns throughout the day. Raising computer monitors to eye level reduces forward head posture, whilst using telephone headsets prevents cervical side-bending during prolonged conversations. Simple changes such as using a timer to prompt regular movement breaks can interrupt prolonged static positioning that contributes to muscle imbalance development.
Educational initiatives focusing on body awareness and movement quality provide individuals with the tools necessary to self-monitor and maintain optimal pelvic alignment. Understanding the relationship between daily activities and pelvic health empowers people to make informed choices about posture, exercise, and lifestyle factors. Regular self-assessment using simple techniques can help identify early warning signs before they progress to symptomatic dysfunction requiring professional intervention.
The economic impact of pelvic dysfunction on healthcare systems worldwide emphasises the critical importance of preventive approaches, with conservative estimates suggesting prevention programmes could reduce treatment costs by up to 40% whilst improving quality of life outcomes.
Workplace wellness programmes incorporating pelvic health education and ergonomic assessments represent cost-effective preventive strategies that benefit both employees and employers. These programmes can reduce absenteeism related to musculoskeletal complaints whilst improving overall workplace productivity. Investment in proper ergonomic equipment and employee education yields significant returns through reduced healthcare costs and improved job satisfaction.
Regular health screening and early intervention protocols can identify pelvic alignment issues before they become symptomatic. Annual postural assessments as part of routine healthcare examinations could detect developing imbalances, allowing for prompt intervention with simple corrective strategies. This proactive approach transforms healthcare delivery from reactive treatment to preventive maintenance, ultimately improving outcomes whilst reducing costs.
Technology integration through smartphone applications and wearable devices offers promising opportunities for real-time posture monitoring and feedback. These tools can provide gentle reminders to adjust posture or take movement breaks, supporting the development of healthier habits throughout the day. However, technology should supplement rather than replace fundamental understanding of proper body mechanics and movement principles.
Community-based exercise programmes specifically designed for pelvic health can provide accessible preventive interventions for diverse populations. Group classes focusing on core stability, hip flexibility, and postural awareness create supportive environments for learning and maintaining healthy movement patterns. These programmes prove particularly valuable for sedentary workers, older adults, and individuals with limited access to individual healthcare services.