Excessive head sweating affects millions of individuals worldwide, often causing significant social discomfort and impacting daily activities. This condition, medically termed craniofacial hyperhidrosis, goes beyond the normal perspiration response to heat or physical exertion. Understanding the complex mechanisms behind cranial sweating patterns can help individuals recognise when their symptoms warrant professional attention and explore appropriate treatment pathways. The intricate network of sweat glands distributed across the scalp and facial regions operates under sophisticated neurological control, making head sweating a particularly challenging condition to manage effectively.
Craniofacial hyperhidrosis: understanding excessive head sweating mechanisms
Craniofacial hyperhidrosis represents a specific manifestation of localised excessive sweating that primarily affects the head, face, and scalp regions. This condition occurs when the body’s thermoregulatory system becomes dysregulated, causing sweat production that far exceeds physiological requirements for temperature control. The sympathetic nervous system, which governs involuntary bodily functions including perspiration, becomes hyperactive in these areas, triggering persistent moisture production even during rest periods or cool environmental conditions.
The prevalence of craniofacial hyperhidrosis varies significantly across populations, with studies indicating that approximately 10% of focal hyperhidrosis cases involve the head and facial regions. Unlike generalised sweating disorders that affect multiple body areas simultaneously, this condition typically presents as isolated cranial perspiration, though it may occasionally coincide with palmar or axillary hyperhidrosis. The severity ranges from mild dampness that becomes noticeable during stress to profuse sweating that drips visibly, creating substantial social and professional challenges for affected individuals.
Research demonstrates that craniofacial hyperhidrosis often manifests differently than other forms of excessive sweating due to the unique anatomical characteristics of head and facial regions. The rich vascular supply and dense nerve innervation patterns in these areas create ideal conditions for amplified sweat responses. Additionally, the inability to conceal facial perspiration, unlike axillary or palmar sweating, intensifies the psychological impact of this condition, often leading to social withdrawal and reduced quality of life measures.
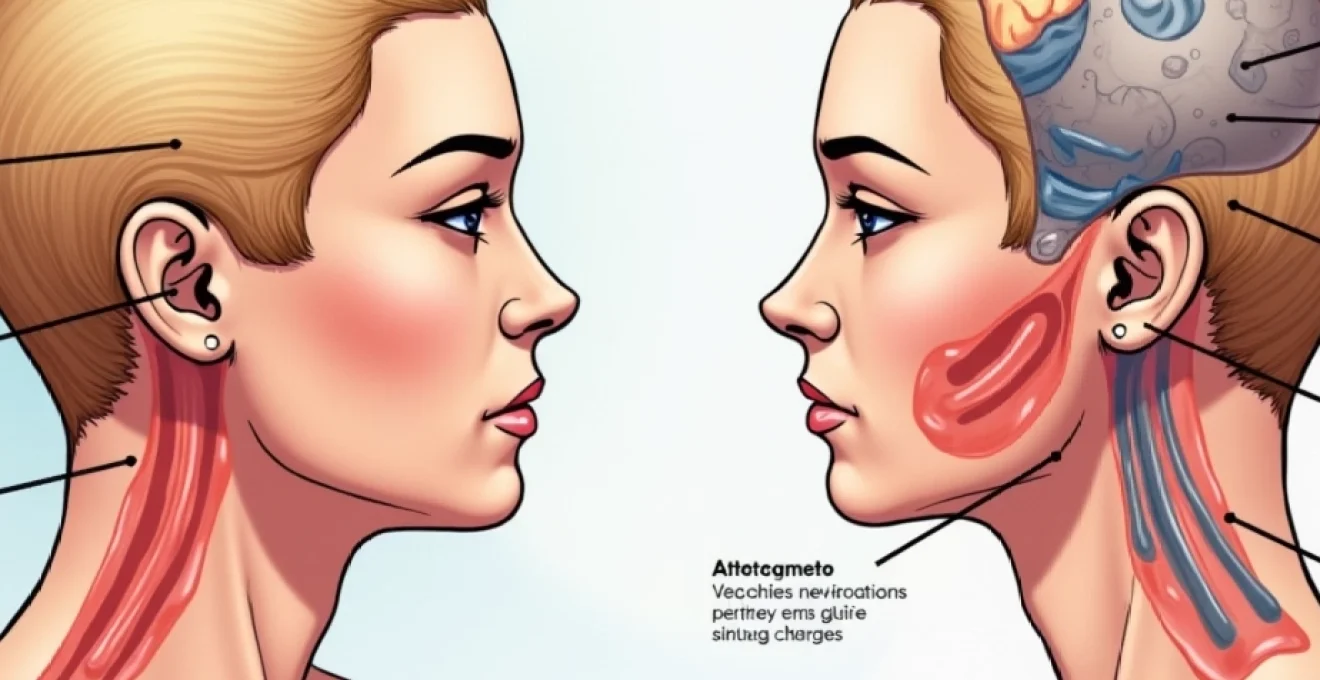
Anatomical structure of cephalic sweat glands and eccrine distribution
The human scalp and facial regions contain an intricate network of sweat glands with varying densities and functional characteristics across different anatomical zones. Understanding this distribution pattern provides crucial insights into why certain individuals experience more pronounced sweating in specific cranial areas. The eccrine sweat glands, responsible for thermoregulatory perspiration, are distributed unevenly across the head, with higher concentrations in the forehead, temporal regions, and upper scalp areas.
Eccrine gland density variations across scalp regions
Eccrine gland density on the scalp demonstrates remarkable regional variation, with the forehead containing approximately 300-400 glands per square centimetre , significantly higher than most other body regions. The temporal areas maintain moderate densities of around 200-250 glands per square centimetre, whilst the posterior scalp regions typically contain 150-200 glands per square centimetre. This uneven distribution explains why many individuals with craniofacial hyperhidrosis report more severe symptoms in frontal head regions compared to the back of the scalp.
Apocrine gland function in forehead and temporal areas
Apocrine sweat glands, though less numerous than eccrine glands in cranial regions, contribute significantly to the overall moisture production and associated odour characteristics. These glands, primarily located in hair follicle-rich areas such as the hairline and temporal regions, produce a protein-rich secretion that becomes malodorous when metabolised by surface bacteria. The interaction between apocrine and eccrine secretions creates the characteristic dampness and potential odour issues experienced by individuals with excessive head sweating.
Sympathetic nervous system innervation patterns
The sympathetic nervous system provides dual innervation to cranial sweat glands through both cholinergic and adrenergic pathways. Cholinergic fibres, utilising acetylcholine as the primary neurotransmitter, directly stimulate eccrine gland activity, whilst adrenergic pathways influence blood flow and indirect glandular function. This complex innervation pattern creates multiple potential points of dysfunction, explaining why craniofacial hyperhidrosis can vary considerably in its presentation and response to different therapeutic interventions.
Sebaceous gland interaction with sweat production
Sebaceous glands, abundant throughout scalp and facial regions, interact significantly with sweat production mechanisms, potentially amplifying the perceived severity of cranial hyperhidrosis. These glands produce sebum, an oily substance that can mix with sweat to create a more noticeable and persistent moisture film on the skin surface. This interaction is particularly pronounced in individuals with naturally oily skin types, who may experience more severe symptoms of head sweating due to the combined effects of sebaceous and eccrine secretions.
Primary focal hyperhidrosis: idiopathic cranial sweating disorders
Primary focal hyperhidrosis affecting the cranial region represents the most common form of excessive head sweating, occurring without identifiable underlying medical conditions or medication triggers. This idiopathic condition typically emerges during childhood or adolescence and persists throughout adult life, though symptom severity may fluctuate with age and environmental factors. The exact pathophysiology remains incompletely understood, though current research points to dysfunction within the sympathetic nervous system’s regulatory mechanisms.
Genetic predisposition and familial clustering patterns
Genetic factors play a substantial role in primary craniofacial hyperhidrosis development, with family history studies revealing inheritance patterns in approximately 65% of affected individuals . This familial clustering suggests autosomal dominant transmission with variable penetrance, though specific genetic mutations responsible for the condition remain largely unidentified. Research indicates that individuals with affected first-degree relatives demonstrate a significantly higher likelihood of developing cranial hyperhidrosis, often with similar anatomical distribution patterns and symptom severity profiles.
Neurotransmitter dysfunction in acetylcholine pathways
Acetylcholine pathway dysfunction represents a key mechanism in primary craniofacial hyperhidrosis, with affected individuals demonstrating heightened sensitivity to cholinergic stimulation. This hypersensitivity manifests as excessive sweat production in response to normal physiological triggers such as emotional stress, mild temperature elevation, or gustatory stimuli. Studies using intradermal acetylcholine challenges consistently demonstrate exaggerated sweat responses in affected cranial regions compared to unaffected body areas and healthy control subjects.
Age-related onset characteristics and progression
Primary craniofacial hyperhidrosis typically manifests during puberty, coinciding with hormonal changes and sympathetic nervous system maturation. The condition often stabilises during early adulthood, though approximately 30% of individuals report symptom improvement after age 40. This age-related progression pattern suggests potential neural plasticity mechanisms that may naturally moderate excessive sweating responses over time, offering hope for individuals experiencing severe symptoms during younger years.
Gender-specific manifestations in craniofacial hyperhidrosis
Gender differences in craniofacial hyperhidrosis presentation reflect complex interactions between hormonal influences, anatomical variations, and social factors. Research indicates that women more frequently report facial sweating symptoms, particularly during hormonal transitions such as menstruation, pregnancy, and menopause. Men typically demonstrate higher rates of scalp hyperhidrosis, possibly related to hair pattern differences and androgen-influenced sebaceous gland activity. These gender-specific patterns influence both symptom perception and treatment response characteristics.
Secondary hyperhidrosis triggers: medical conditions affecting cephalic sweating
Secondary hyperhidrosis affecting cranial regions results from identifiable medical conditions, medications, or physiological states that disrupt normal thermoregulatory mechanisms. Unlike primary hyperhidrosis, secondary forms often present with additional systemic symptoms and may develop suddenly in previously unaffected individuals. Recognising these underlying triggers becomes crucial for appropriate treatment selection, as addressing the root cause frequently resolves excessive sweating symptoms more effectively than symptomatic management alone.
Thyroid dysfunction and Hyperthyroidism-Induced perspiration
Hyperthyroidism represents one of the most common endocrine causes of secondary craniofacial hyperhidrosis, affecting the metabolic processes that regulate heat production and dissipation. Elevated thyroid hormone levels accelerate cellular metabolism, generating excess heat that triggers compensatory sweating responses throughout the body, including prominent cranial regions. Studies demonstrate that approximately 85% of hyperthyroid patients experience excessive sweating, with facial and scalp regions frequently affected due to their rich vascular supply and high eccrine gland density.
Menopause-related hormonal fluctuations and hot flashes
Menopausal hormonal changes create significant disruptions in thermoregulatory control, leading to characteristic hot flashes that frequently manifest as intense cranial sweating episodes. The declining oestrogen levels affect hypothalamic temperature regulation centres, creating a narrowed thermoneutral zone that triggers sweating responses to minimal temperature elevations. These vasomotor symptoms typically begin with facial flushing and progress to profuse head and neck perspiration, affecting up to 75% of menopausal women for periods ranging from months to several years.
Diabetes mellitus complications and autonomic neuropathy
Diabetic autonomic neuropathy can produce paradoxical sweating patterns, including compensatory cranial hyperhidrosis when peripheral sweating mechanisms become impaired. This condition develops gradually in individuals with poorly controlled diabetes mellitus, affecting the sympathetic nerve fibres that regulate sweat gland function. The resulting asymmetric sweating patterns often concentrate in upper body regions, including the head and face, as the nervous system attempts to maintain thermoregulatory function through unaffected neural pathways.
Medication-induced diaphoresis from SSRIs and Beta-Blockers
Selective serotonin reuptake inhibitors (SSRIs) commonly cause secondary hyperhidrosis as an adverse effect, with cranial sweating frequently reported among affected patients. These medications alter neurotransmitter balance in ways that can stimulate excessive sweat production, particularly during sleep periods or emotional stress. Similarly, certain beta-blockers paradoxically increase sweating in some individuals, despite their intended cardiovascular effects. Medication-induced diaphoresis typically develops within weeks of treatment initiation and may persist throughout therapy duration.
Neurological disorders: parkinson’s disease and multiple sclerosis
Progressive neurological conditions such as Parkinson’s disease and multiple sclerosis can disrupt normal autonomic function, leading to secondary craniofacial hyperhidrosis patterns. Parkinson’s disease affects dopaminergic pathways that influence thermoregulatory control, whilst multiple sclerosis lesions may directly impact sympathetic nervous system function. These neurological causes of excessive sweating often present alongside other autonomic symptoms and typically require specialised neurological management approaches rather than conventional hyperhidrosis treatments.
Environmental and lifestyle factors exacerbating cranial perspiration
Environmental conditions and lifestyle choices significantly influence the severity and frequency of cranial sweating episodes, even in individuals without underlying hyperhidrosis conditions. Understanding these modifiable factors enables targeted interventions that can substantially reduce symptom burden and improve quality of life. Temperature regulation, dietary influences, stress management, and clothing choices all play crucial roles in determining the extent of head sweating responses.
Ambient temperature and humidity levels create the primary environmental triggers for cranial perspiration, with high humidity conditions particularly problematic as they impair the body’s natural evaporative cooling mechanisms. When environmental humidity exceeds 70% , sweat evaporation rates decrease dramatically, leading to accumulation of moisture on skin surfaces and the perception of increased sweating. This effect becomes amplified in cranial regions due to hair coverage that further restricts air circulation and heat dissipation.
Dietary factors contribute significantly to cranial sweating patterns, with certain foods and beverages acting as gustatory triggers for excessive perspiration. Spicy foods containing capsaicin stimulate trigeminal nerve pathways that can activate facial sweating responses, whilst caffeine consumption increases sympathetic nervous system activity and overall heat production. Hot beverages and alcohol consumption create additional thermal burdens that frequently manifest as cranial sweating, particularly in sensitive individuals.
Environmental modifications and lifestyle adjustments can reduce cranial sweating by up to 40% in many individuals, making these interventions crucial first-line management strategies.
Psychological stress represents a major lifestyle factor influencing cranial hyperhidrosis severity, as emotional responses directly activate sympathetic nervous system pathways controlling sweat production. Chronic stress states maintain elevated baseline sympathetic tone, making individuals more susceptible to sweating triggers and reducing their physiological threshold for perspiration responses. Stress management techniques including meditation, regular exercise, and adequate sleep patterns can significantly improve symptom control and reduce the frequency of severe sweating episodes.
Occupational and recreational activities that involve sustained mental concentration or physical exertion in warm environments create compounding effects that exacerbate cranial sweating. Individuals working in high-stress professions or engaging in activities requiring protective headwear often experience worsening symptoms due to restricted ventilation and increased local temperatures. Strategic timing of activities and environmental modifications can help minimise these occupational triggers whilst maintaining professional and personal commitments.
Clinical assessment and diagnostic protocols for head sweating
Comprehensive clinical evaluation of excessive cranial sweating requires systematic assessment to differentiate primary hyperhidrosis from secondary causes and determine appropriate treatment strategies. Healthcare providers utilise structured diagnostic protocols that evaluate symptom patterns, medical history, physical examination findings, and specialised testing when indicated. This thorough approach ensures accurate diagnosis and guides evidence-based treatment selection tailored to individual patient needs.
The initial clinical assessment begins with detailed symptom characterisation, including onset timing, anatomical distribution, trigger identification, and severity grading using standardised scales. Patients typically undergo questioning about family history, medication use, associated symptoms, and functional impact on daily activities. This history-taking process helps distinguish primary focal hyperhidrosis, which typically begins during adolescence and affects specific body regions, from secondary forms that may develop at any age and often present with systemic symptoms.
Physical examination focuses on identifying signs of underlying medical conditions that might cause secondary hyperhidrosis whilst documenting the extent and characteristics of cranial sweating. Healthcare providers assess thyroid gland size and function, evaluate neurological status, and examine affected skin areas for signs of chronic moisture exposure such as maceration or secondary infections. Vital sign assessment and cardiovascular examination help identify potential systemic causes requiring specific medical management.
Accurate diagnosis of cranial hyperhidrosis requires comprehensive evaluation that considers both primary and secondary causes, as treatment approaches differ significantly between these categories.
Laboratory investigations may include thyroid function tests, glucose metabolism assessment, and complete blood count to screen for common secondary causes of excessive sweating. Advanced testing such as thermoregulatory sweat testing or quantitative sudomotor axon reflex testing becomes necessary in complex cases where neurological causes are suspected. These specialised assessments provide objective measurements of sweat production rates and help localise dysfunction within the sympathetic nervous system pathways.
Diagnostic imaging studies are rarely required for primary craniofacial hyperhidrosis but may become necessary when secondary neurological causes are suspected. Magnetic resonance imaging of the brain or cervical spine can identify structural abnormalities affecting autonomic function, whilst computed tomography may be indicated for suspected malignancies causing paraneoplastic sweating syndromes. The decision to pursue advanced imaging depends on clinical presentation and the presence of additional neurological symptoms.
Treatment planning requires careful consideration of symptom severity, patient preferences, contraindications to specific therapies, and realistic outcome expectations. Healthcare providers typically begin with conservative management approaches including topical antiperspirants and lifestyle modifications before progressing to more invasive interventions such as botulinum toxin injections or oral medications. The goal becomes achieving optimal symptom control whilst minimising treatment-related side effects and maintaining patient quality of life throughout the management process.