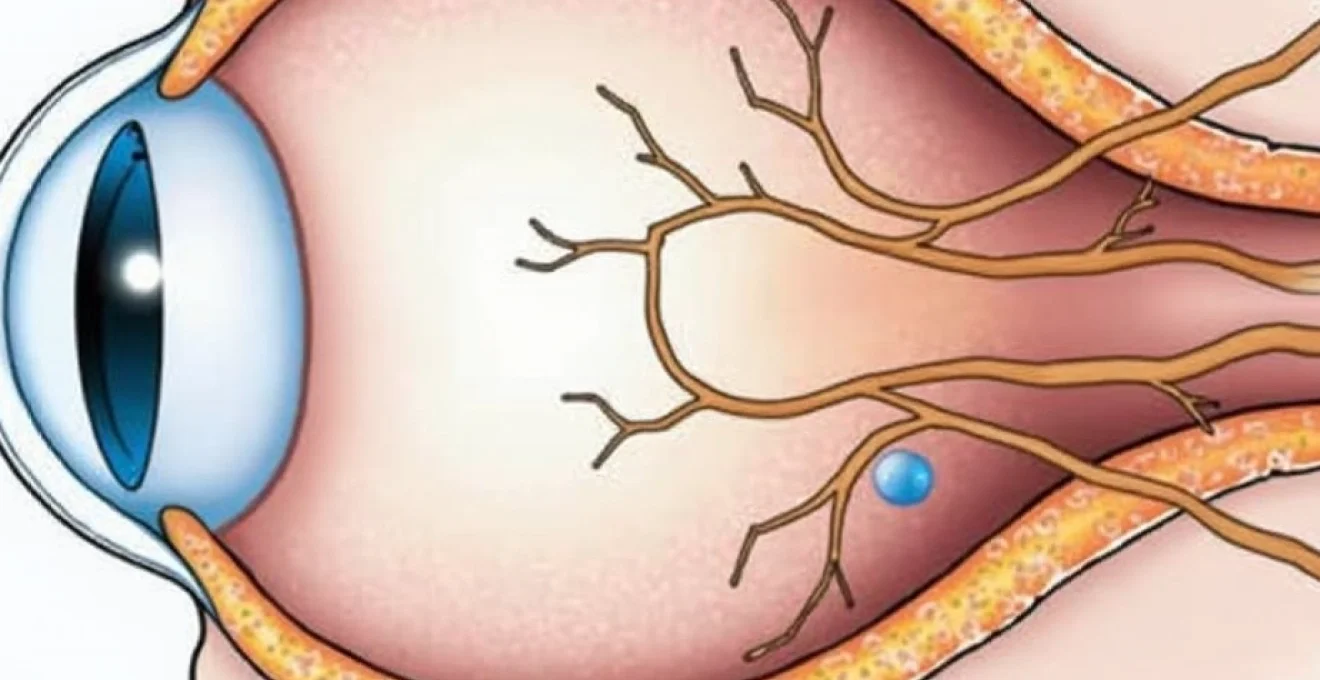
Retrobulbar tumours, those positioned behind the eyeball within the orbital cavity, present some of the most complex challenges in neurosurgical practice. These space-occupying lesions can arise from various anatomical structures including the optic nerve, extraocular muscles, orbital fat, or extend from adjacent regions such as the brain or sinuses. The delicate nature of orbital anatomy, combined with the critical importance of preserving vision and ocular function, demands exceptional surgical precision and expertise. Modern neurosurgical techniques have revolutionised the approach to these challenging cases, offering patients improved outcomes whilst minimising the risk of visual complications.
Retrobulbar tumour classification and diagnostic assessment
Understanding the precise nature of a retrobulbar tumour is fundamental to determining the most appropriate surgical strategy. The classification system encompasses both benign and malignant lesions, with each category requiring distinct therapeutic approaches. Benign tumours typically grow slowly and exert pressure on surrounding structures through mass effect, whilst malignant lesions may demonstrate invasive characteristics that complicate surgical planning. The diagnostic process begins with a comprehensive clinical evaluation, including detailed visual field testing and ophthalmological examination to assess the extent of functional impairment.
Advanced imaging techniques form the cornerstone of preoperative assessment, providing surgeons with detailed three-dimensional understanding of tumour location, size, and relationship to critical structures. Magnetic resonance imaging with gadolinium enhancement offers superior soft tissue contrast, enabling precise delineation of tumour margins and identification of potential vascular involvement. Computed tomography remains valuable for evaluating bony structures and calculating precise measurements for surgical planning. The integration of multiple imaging modalities creates a comprehensive roadmap for the surgical team, reducing operative risks and improving patient outcomes.
Primary orbital tumours: meningiomas and optic nerve gliomas
Primary orbital meningiomas represent approximately 2% of all meningiomas but constitute a significant proportion of retrobulbar tumours. These lesions typically arise from the optic nerve sheath or sphenoid wing, gradually compressing neural structures and causing progressive visual deterioration. Optic nerve gliomas, more commonly encountered in paediatric populations, demonstrate varying degrees of aggressiveness and may extend intracranially. The surgical approach to these tumours requires careful consideration of the potential for visual preservation versus the need for complete resection.
Secondary metastatic lesions from breast and lung carcinomas
Metastatic deposits to the orbital region frequently originate from breast, lung, and prostate malignancies. These secondary tumours often present with rapid onset symptoms due to their aggressive growth patterns and tendency to invade surrounding tissues. The surgical management of metastatic orbital disease must be carefully balanced against the patient’s overall oncological status and life expectancy. Palliative surgical intervention may be considered when tumours cause significant pain, visual impairment, or cosmetic deformity that impacts quality of life.
Vascular malformations: cavernous haemangiomas and arteriovenous malformations
Cavernous haemangiomas represent the most common benign orbital tumour in adults, typically presenting as well-encapsulated lesions that can be safely removed with minimal risk to surrounding structures. These vascular malformations rarely demonstrate malignant transformation but may cause progressive proptosis and visual field defects through mass effect. Arteriovenous malformations, whilst less common, pose greater surgical challenges due to their complex vascular architecture and potential for significant bleeding during manipulation.
Advanced imaging protocols: MRI with gadolinium and CT angiography
Contemporary imaging protocols employ sophisticated techniques to maximise diagnostic accuracy and surgical planning effectiveness. High-resolution magnetic resonance imaging with multiple sequences provides detailed anatomical information, whilst dynamic contrast enhancement reveals vascular characteristics and tumour perfusion patterns. CT angiography proves particularly valuable when vascular involvement is suspected, offering three-dimensional reconstruction of arterial and venous anatomy. These advanced imaging modalities enable surgical teams to anticipate potential complications and develop contingency plans for complex cases.
Surgical access routes and anatomical considerations
The selection of an appropriate surgical approach depends on multiple factors including tumour location, size, histological type, and relationship to critical neurovascular structures. Each access route offers distinct advantages and limitations, requiring careful consideration of the risk-benefit profile for individual patients. The orbital cavity’s confined space and proximity to vital structures necessitate meticulous surgical planning and execution to achieve optimal outcomes whilst preserving function.
The key to successful retrobulbar tumour surgery lies in selecting the most appropriate approach that provides adequate exposure whilst minimising trauma to healthy tissues.
Modern surgical techniques emphasise minimally invasive approaches whenever possible, utilising advanced visualisation technologies and microsurgical instruments to reduce operative morbidity. The evolution of surgical approaches has been driven by improved understanding of orbital anatomy and the development of sophisticated surgical instruments designed specifically for work in confined spaces. Patient positioning, anaesthetic considerations, and intraoperative monitoring protocols all contribute to the overall safety and effectiveness of the procedure.
Lateral orbitotomy via kronlein’s approach
The lateral orbitotomy approach, first described by Kronlein in 1888, remains a cornerstone technique for accessing retrobulbar tumours located in the lateral and posterior orbital compartments. This approach involves creating a curved incision along the lateral orbital rim, followed by careful dissection through tissue planes to reach the orbital cavity. The zygomatic bone removal provides excellent visualisation of the lateral orbital contents whilst preserving important neurovascular structures. Modern modifications of this technique incorporate endoscopic assistance and improved reconstructive methods to optimise both functional and cosmetic outcomes.
Superior orbitotomy through frontotemporal craniotomy
Superior orbital access through a frontotemporal craniotomy provides optimal exposure for tumours located in the superior orbital compartment or those extending intracranially. This approach allows simultaneous management of both orbital and intracranial components of complex lesions, particularly relevant for large meningiomas or extensive gliomas. The superior approach offers excellent visualisation of the optic nerve and superior orbital structures, enabling precise microsurgical dissection whilst maintaining adequate haemostatic control.
Transcranial pterional approach for sphenoid wing meningiomas
The pterional approach represents the gold standard for accessing sphenoid wing meningiomas with orbital extension. This technique provides wide exposure of the middle cranial fossa and superior orbital fissure, allowing complete tumour removal whilst preserving critical neurovascular structures. The approach requires careful planning to ensure adequate bone removal and optimal angle of attack for tumour visualisation. Reconstruction of the orbital roof and lateral wall may be necessary to prevent pulsatile exophthalmos and maintain proper globe position.
Endoscopic endonasal resection for medial orbital wall tumours
Endoscopic endonasal approaches have gained popularity for selected retrobulbar tumours, particularly those involving the medial orbital wall or extending from the ethmoid sinuses. This minimally invasive technique avoids external incisions and reduces postoperative morbidity whilst providing excellent visualisation of the surgical field. The endoscopic approach requires specialised instrumentation and expertise in endonasal anatomy, but offers significant advantages in terms of cosmetic outcomes and recovery time for appropriately selected cases.
Microsurgical techniques and intraoperative monitoring
The successful removal of retrobulbar tumours relies heavily on advanced microsurgical techniques and comprehensive intraoperative monitoring systems. These technologies enable surgeons to operate with unprecedented precision whilst continuously assessing the functional integrity of critical structures. The integration of multiple monitoring modalities provides real-time feedback that guides surgical decision-making and helps prevent iatrogenic injury to vital neural and vascular structures.
Modern operating theatres equipped with state-of-the-art technology have transformed the landscape of orbital surgery, offering surgeons enhanced visualisation and improved safety profiles. The combination of high-powered surgical microscopes, neuronavigation systems , and sophisticated monitoring equipment creates an environment where complex procedures can be performed with confidence and precision. These technological advances have contributed significantly to improved patient outcomes and reduced complication rates in retrobulbar tumour surgery.
Neuronavigation systems: stealth station and BrainLab integration
Neuronavigation technology has revolutionised the precision of retrobulbar tumour surgery, providing surgeons with real-time three-dimensional guidance based on preoperative imaging studies. The Stealth Station and BrainLab systems offer millimetre accuracy in localising tumours and critical structures, reducing the risk of inadvertent damage to healthy tissues. These systems enable surgeons to plan optimal approaches and track instrument positions throughout the procedure, enhancing both safety and efficacy of tumour removal.
Intraoperative ultrasound for Real-Time tumour localisation
Intraoperative ultrasound provides dynamic imaging capabilities that complement static neuronavigation data, allowing surgeons to visualise tissue changes and brain shift that occur during the procedure. This technology proves particularly valuable when dealing with cystic or heterogeneous tumours that may change configuration during surgical manipulation. Real-time ultrasound guidance enables precise targeting of residual tumour tissue and helps confirm complete resection whilst minimising damage to surrounding healthy structures.
Visual evoked potential monitoring during optic nerve manipulation
Visual evoked potential monitoring represents a critical safety measure during procedures involving close proximity to the optic nerve or visual pathways. This technique provides continuous assessment of visual function throughout the procedure, alerting the surgical team to potential compromise of visual pathways before permanent damage occurs. The integration of VEP monitoring into surgical protocols has significantly improved the safety profile of complex orbital procedures and contributed to better preservation of postoperative visual function.
Frozen section analysis for immediate histopathological confirmation
Intraoperative frozen section analysis enables immediate histopathological diagnosis and guides surgical decision-making in real-time. This technique proves particularly valuable when dealing with lesions of uncertain aetiology or when the extent of resection depends on tumour type. Rapid pathological assessment allows surgeons to modify their approach based on definitive tissue diagnosis, ensuring appropriate treatment whilst minimising unnecessary tissue removal for benign conditions.
Post-operative management and rehabilitation protocols
The postoperative period following retrobulbar tumour removal requires careful monitoring and structured rehabilitation to optimise functional outcomes and prevent complications. Immediate postoperative care focuses on managing pain, monitoring for signs of bleeding or infection, and assessing neurological function. The complexity of orbital anatomy necessitates specialised nursing care and close collaboration between neurosurgical, ophthalmological, and rehabilitation teams to ensure comprehensive patient management.
Early mobilisation and graduated activity protocols help prevent complications such as deep vein thrombosis whilst promoting optimal healing. Pain management strategies must balance adequate analgesia with the need to monitor neurological function, often requiring multimodal approaches that minimise opioid dependence. Wound care protocols specific to orbital surgery address the unique challenges of managing incisions in areas subject to frequent movement and potential contamination from tear film and nasal secretions.
Visual rehabilitation following retrobulbar tumour surgery may require extensive therapy to maximise functional outcomes and help patients adapt to any residual visual deficits. Occupational therapy assessment and intervention can prove invaluable in helping patients develop strategies for managing activities of daily living with altered visual function. The multidisciplinary approach to postoperative care ensures that all aspects of recovery are addressed comprehensively, from immediate surgical concerns to long-term functional adaptation.
Successful outcomes in retrobulbar tumour surgery depend not only on technical surgical skill but also on comprehensive postoperative care and rehabilitation programmes tailored to individual patient needs.
Follow-up protocols typically involve serial imaging studies to monitor for tumour recurrence and assess healing of surgical sites. The frequency and duration of follow-up depend on tumour histology, completeness of resection, and individual patient factors. Long-term surveillance may reveal delayed complications or functional changes that require intervention, emphasising the importance of maintaining regular contact with the surgical team throughout the recovery period.
Long-term visual outcomes and complications management
The long-term visual outcomes following retrobulbar tumour removal depend on multiple factors including tumour type, size, location, and preoperative visual function. Patients with benign tumours and intact preoperative vision generally demonstrate the best outcomes, whilst those with malignant lesions or significant preoperative visual impairment may experience persistent deficits. The management of complications requires ongoing collaboration between neurosurgical and ophthalmological teams to address both structural and functional issues that may arise.
Common complications following retrobulbar tumour surgery include diplopia, ptosis, enophthalmos, and various degrees of visual field defects. The incidence and severity of these complications vary according to the surgical approach employed and the extent of tissue manipulation required for tumour removal. Early recognition and appropriate management of complications can often prevent progression to more severe functional impairment and improve overall patient satisfaction with surgical outcomes.
Reconstructive procedures may be necessary to address structural abnormalities resulting from extensive tumour removal or complications of the initial surgery. These may include orbital floor reconstruction, extraocular muscle repair, or eyelid repositioning procedures to restore both function and appearance. The timing of reconstructive interventions must be carefully planned to allow adequate healing of the primary surgical site whilst addressing functional concerns that impact quality of life.
Patient education plays a crucial role in managing expectations and promoting optimal outcomes following retrobulbar tumour surgery. Understanding the potential for gradual improvement in visual function over months to years can help patients maintain realistic expectations and comply with rehabilitation programmes. Regular assessment of visual function using standardised testing protocols enables objective monitoring of recovery and identification of patients who might benefit from additional interventions.
Radiotherapy integration: stereotactic radiosurgery and proton beam therapy
The integration of radiotherapy techniques with surgical management has expanded treatment options for patients with retrobulbar tumours, particularly those with lesions that cannot be completely resected or demonstrate high risk for recurrence. Stereotactic radiosurgery offers precise targeting of residual tumour tissue whilst sparing adjacent healthy structures, making it an attractive adjuvant treatment option for carefully selected cases. The decision to incorporate radiotherapy must consider tumour histology, patient age, and the potential for radiation-induced complications affecting visual function.
Proton beam therapy represents an advanced form of radiation treatment that offers superior dose distribution characteristics compared to conventional photon therapy. This technology enables delivery of high doses to tumour tissue whilst significantly reducing radiation exposure to critical structures such as the optic nerve, retina, and brain stem. The availability of proton therapy facilities remains limited, but outcomes data suggest significant advantages for selected orbital tumours, particularly in paediatric populations where minimising late effects is paramount.
The combination of precision surgery and advanced radiotherapy techniques offers patients the best opportunity for tumour control whilst preserving visual function and quality of life.
Treatment planning for radiotherapy following orbital surgery requires sophisticated imaging fusion techniques and close collaboration between radiation oncologists, neurosurgeons, and medical physicists. The development of individualised treatment plans must account for surgical changes in anatomy and the presence of implanted materials that may affect dose distribution. Quality assurance protocols ensure accurate delivery of prescribed radiation doses whilst maintaining the highest safety standards throughout the treatment course.
Long-term follow-up following combined surgical and radiation treatment requires monitoring for both tumour control and treatment-related complications. Radiation-induced changes in surrounding tissues may develop months to years following treatment, necessitating ongoing surveillance and potential intervention. The expertise required for managing these complex cases emphasises the importance of treatment at specialised centres with experience in both surgical and radiation oncology aspects of orbital tumour management.